
In January, 2009, a thirty-one-year-old prostitute visited a clinic in Kyoto, Japan, for a routine checkup. Because sex workers are so likely to acquire sexually transmitted diseases, many have themselves checked for infections even in the absence of symptoms. Indeed, although the woman displayed no outward signs of gonorrhea, her lab test came back positive; she carried the gonococcus microbe in her throat, a common reservoir. After a second visit, doctors at the clinic gave her an injection of ceftriaxone, an antibiotic considered by infectious-disease experts to be the definitive treatment for gonorrhea. It didn’t work; two weeks later, when she returned to the clinic, a throat culture again tested positive. She was given another dose, but it, too, failed, and, at first, doctors assumed that she had been newly infected. Now, however, public-health experts view the Kyoto case as something far more alarming: the emergence of a strain of gonorrhea that is resistant to the last drug available against it, and the harbinger of a sexually transmitted global epidemic. “The microbe appears to be emerging as a superbug,” Dr. Magnus Unemo, the head of the World Health Organization’s Collaborating Center for Gonorrhea and Other Sexually Transmitted Infections, in Sweden, told me recently. “This is what we have feared for many years.”
Gonorrhea is the second most commonly reported infectious disease in the United States, after chlamydia. More than three hundred thousand new cases are reported each year to the Centers for Disease Control, although the actual incidence is probably twice as high. A hundred million annual cases are estimated worldwide. Symptoms, when they occur, are very painful: swelling and a burning sensation in the urethra or the urinary tract, often accompanied by the release of pus. Untreated, gonorrhea in men can lead to scarring of the urethra and, eventually, to epididymitis, a painful condition of the testicles that can result in sterility. In women, the infection can migrate from the cervix into the uterus and the fallopian tubes, causing pelvic inflammatory disease and infertility. Infants born to mothers with gonorrhea can contract the infection in the eye and become blind. In some cases, among both men and women, the microbe enters the bloodstream, infecting the joints, the skin, the heart valves, and even the brain; it also increases one’s susceptibility to H.I.V. Remarkably, more than fifty per cent of women infected with gonorrhea display no symptoms at all; they carry and transmit it unaware. While gonorrhea in the throat may cause soreness, ninety per cent of throat infections, like the Kyoto case, produce no symptoms whatsoever.
Gonorrhea has been recognized since antiquity. The second-century physician Galen, mistaking pus for semen, derived the name from the Greek words gonos (“seed”) and rhoia (“flow”). In the time of the Tudors, gonorrhea was called “the clap,” a term that was still in use when, in 1760, at the age of nineteen, James Boswell, the journalist and the biographer of Samuel Johnson, was first infected by a London prostitute. He apparently contracted the disease at least a dozen more times; the infection spread to his testicles and prostate and scarred his urinary tract. (In his diary, he referred to his malady as “Signor Gonorrhea” and “a memorandum of vice.”) He died, at fifty-four, of kidney failure brought on, some medical historians believe, by complications from the disease. In 1901, the New York City medical examiner, the founder of a “social hygiene” movement, estimated that eighty of a hundred men in the city had contracted gonorrhea at some point in their lives.
Cures ranged from the absurd to the excruciating. At various times, Boswell tried bloodletting, a low-calorie diet, and a daily bottle of Kennedy’s Lisbon Diet Drink, which cost a lot, contained mostly sarsaparilla, and did nothing. In some cases, a doctor might use a thin tube to open the blocked urethra and, with a syringe, inject a solution of vitriol—sulfuric acid—or salt solutions made with mercury or lead, which over time could do as much damage as the disease. The historian Allan Brandt describes a cure proposed by one physician for chordee, a complication of gonorrhea that causes the head of the penis to curve downward. The affected member, the physician wrote, should be placed “with the curve upward on a table and struck a violent blow with a book . . . and so flattening it.”
In the nineteen-thirties, antibiotics changed the clinical picture of gonorrhea and other sexually transmitted diseases, and, with it, social attitudes. Once feared for its devastating complications, gonorrhea was now viewed as a bothersome but temporary price to pay for sexual freedom. The sexual revolution of the nineteen-sixties ushered in rising rates of gonorrhea, as condoms, which effectively prevent transmission, were abandoned in favor of oral contraceptives. Only after the risk of death from AIDS began to increase, in the nineteen-eighties, did condom use again become a norm. A federally funded gonorrhea-control program, started in 1972, perhaps made a difference; by 1997, the number of yearly cases of gonorrhea reported to the C.D.C. had fallen by nearly three-quarters compared with its peak, in 1975. In 2009, the number of gonorrhea cases in the U.S. was at an all-time low. “Ten or fifteen years ago, we thought it was going to be eradicated in some Western countries,” Unemo told me.
But as modern medicine has adapted so has the microbe. Natural selection has given rise to strains of the bacterium that are resistant, in varying degrees, to some or all of the treatments applied to them—sulfa drugs, penicillin, tetracyclines, fluoroquinolones, and macrolides. Now only one class of drugs, called cephalosporins—cefixime, a tablet, and ceftriaxone, administered by injection—is known to reliably treat it, and for several years resistance to cefixime has been rising. (In the lab, resistance is measured by testing how susceptible the microbe is to various concentrations of a drug.) Between 2000 and 2010, the number of cases of decreased cefixime susceptibility in California and Hawaii rose from zero per cent to more than four per cent and seven per cent, respectively, probably as a result of traffic from Asia, where cefixime resistance is more widespread. Five per cent is cause for concern; in August, the C.D.C. recommended phasing out cefixime nationwide and, instead, treating gonorrhea with a combination of ceftriaxone and either azithromycin or doxycycline. According to a recent British report, last year eleven per cent of isolates of the microbe showed reduced susceptibility to cefixime; among gay men, the figure is seventeen per cent.
“We are seeing decreased sensitivity to cefixime in all twenty-one countries in Europe,” Dr. Catherine Ison, a researcher in the U.K.’s surveillance program for sexually transmitted infections, told me. “It’s worrying.”
The Kyoto case, in 2009, marked the appearance of a microbial strain that was resistant to ceftriaxone—the first instance of broad resistance. In June, 2010, a second case emerged, in France; a third appeared in Sweden in July of that year, in a man who had recently had protected vaginal sex and unprotected oral sex with a casual partner in Japan. A fourth case occurred in Slovenia last September, and a fifth and sixth in Spain this past May. All appear to be descendants of a single cefixime-resistant strain, and they “are probably only the tip of the iceberg,” Unemo said. “Japan has been the epicenter for their emergence, and now these antibiotic-resistant gonococcal clones are spreading.” No cases have yet been reported in the U.S., but resistant gonorrhea is likely to arrive and spread long before physicians and the C.D.C. recognize it; some public-health officials predict that in five to eight years the superbug will be widespread. Whatever freedoms were won during the sexual revolution, bacterial evolution promises soon to constrain.
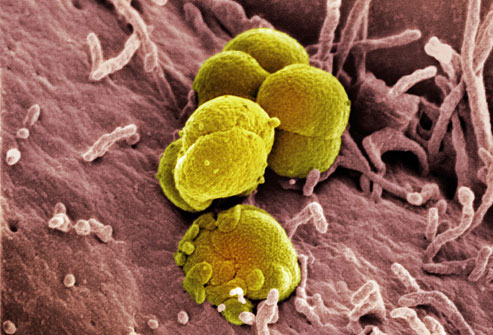
Under the microscope, Neisseria gonorrhoeae looks like buckshot—small, round bacteria that tend to form pairs. The microbe carries specialized proteins that help it attach firmly to the surface of cells and other proteins that blunt a host’s immune-system response and prevent white blood cells from ingesting and degrading it. Together, these tools grant the gonococcus the ability to fasten to and invade the cells that line the human urethra, cervix, rectum, and throat, and the lining of the eyelid and eye.
In some respects, N. gonorrhoeae is a fragile organism; dry conditions, changes in temperature, and the ultraviolet rays in sunlight destroy it. As a result, it is transmitted only through intimate contact with body fluids; it doesn’t thrive on inanimate objects and can’t be picked up from toilet seats. Yet it is far more contagious than H.I.V. A woman who has unprotected sex with an H.I.V.-infected man has roughly a one-in-a-thousand chance of contracting the virus. The transmission rate among gay men having anal sex is an order of magnitude higher, about one in a hundred. In contrast, with gonorrhea a man has a twenty-five-per-cent chance of catching the microbe from an infected partner. For women, the odds are as high as sixty-six per cent.
Gonorrhea is commonly thought of as a painful genital infection. But the microbe also grows robustly in the pharynx, at the back of the throat. With hairlike structures that extend from the cell surface, it scavenges DNA that has been cast loose by the death or dissolution of other microbes, and incorporates them into its own genome. This turns out to be a highly efficient way of acquiring resistance to antibiotics. Multiplying in the pharynx, the gonococcus regularly encounters infectious microbes; these include other strains of antibiotic-resistant gonorrhea and unrelated microbes that have accumulated mutations to withstand antibiotics of the kind taken indiscriminately for sore throats and other ailments. A 2011 study by researchers in Japan contends that the Kyoto strain acquired its resistance to ceftriaxone in the pharynx, from other bacteria of the Neisseria family that live there.
In effect, the human pharynx is a spawning ground for resistance. “Neisseria gonorrhoeae is just infinitely mutable,” Dr. Katherine Hsu, an infectious-disease expert and the medical director of the S.T.D. Prevention Division at the Massachusetts Department of Public Health, told me. The throat, she said, is where “the gonococcus is having sex, so to speak, with other bacteria.” And, because pharyngeal gonorrhea rarely produces symptoms, it is more likely both to go untreated and to be passed on unknowingly.
A driving factor behind the rise in gonorrhea infections, as well as the trend toward total antibiotic resistance, is our complacent attitude toward oral sex. Saliva contains enzymes that destroy gonorrhea, so kissing and cunnilingus don’t spread it. But fellatio, which brings the tip of the urethra near the pharynx, carries a high risk of infecting one partner or the other. According to Dr. Peter Rice, a gonorrhea expert at the University of Massachusetts Medical School in Worcester, fellatio “is the only predictable way to transmit gonococcal infection to the pharynx.”
In many circles, however, especially since the era of H.I.V., oral sex has been embraced as a safe alternative to intercourse. In August, the C.D.C. reported that, of more than six thousand teens interviewed between 2007 and 2010, nearly half said that they had experienced oral sex; the study’s authors concluded that “adolescents perceive fewer health-related risks for oral sex compared with vaginal intercourse.” Recent statistics from Los Angeles County suggest that the proportion of pharyngeal to genital gonorrhea cases among adolescents has increased sevenfold since 1988. “This represents a change in sexual practices in American youth and may provide antimicrobial-resistant gonococci an added advantage,” Rice told me.
The emerging drug-resistant strains of gonorrhea are most common among commercial sex workers and men who have sex with men, perhaps because these groups are more likely to be infected repeatedly. But the wider picture is more complex. In the U.S., gonorrhea in general is linked to poverty and youth; it is far more common among blacks than among whites, and men and women between the ages of fifteen and twenty-four make up the largest percentage of cases. According to the C.D.C., adolescents and young adults account for nearly half of all new cases of sexually transmitted disease, even though the group represents just twenty-five per cent of the sexually active population. The adaptive nature of the gonococcus, coupled with the prevalence of unprotected oral sex, all but insures that drug-resistant gonorrhea will eventually take root in the general heterosexual population. Unemo warned, “When you get into the population of young heterosexuals, it can very quickly spread.”
The progression of a disease like AIDS is straightforward: in the absence of drugs, it kills. Gonorrhea produces a subtler array of outcomes. Even without antibiotics, most people who contract gonorrhea will recover spontaneously, as their immune systems eliminate the microbe. This can take weeks or months; in the meantime, the infection can damage vital tissues, causing scarring and a painful stricture of the urethra in men and pelvic inflammatory disease in women. James Boswell, like many in his situation, often found that if he abstained from sex for a few weeks his condition cleared up by itself. Unemo posits that the Japanese prostitute who tested positive in 2009 for ceftriaxone-resistant gonorrhea naturally fought off the infection after several months, perhaps without experiencing any symptoms.
Effective antibiotics can eliminate the microbe within hours. The surest defense against cephalosporin-resistant gonorrhea would be a new antibiotic, but there are no commercially available treatments to take the place of ceftriaxone. The economics of drug development favor daily medications that are taken for long periods—such as Lipitor, for high cholesterol, and Prozac, for depression—over antibiotics that are typically prescribed for only days or weeks. As a result, efforts to develop new antibiotics against superbugs have been all but abandoned by most major pharmaceutical companies. “We’re down to the last class of antibiotics known to treat gonorrhea,” Dr. Gail Bolan, the director of the Division of S.T.D. Prevention at the C.D.C., told me. In February, Bolan was among the authors of an article in the New England Journal of Medicine that alerted the clinical community to the threat of resistant gonorrhea. A bill, called the GAIN Act, has been introduced in Congress that would speed up the approval of new antibiotics, to encourage drug companies to join the fight. At least one study at the National Institutes of Health is investigating whether combinations of existing drugs might have the ability to treat ceftriaxone-resistant gonorrhea. But such solutions may be years away, Bolan said.
Scientists likewise have made little progress in developing a vaccine that would gird the human immune system against a gonococcus infection. The challenge is daunting, Dr. Fred Sparling, an infectious-disease researcher at the University of North Carolina who has labored for years to develop a gonorrhea vaccine, told me. Although the body can gradually clear gonorrhea on its own, most people are easily reinfected, which suggests that whatever immune response occurs the first time does not last for long. In experiments where healthy male volunteers were infected with gonorrhea, the subjects showed no sign of an increased resistance to a second infection—such as a rise in the number of antibodies—even when the second infection followed within just two weeks of treatment of the first. A vaccine trial among high-risk U.S. military personnel stationed in Korea was equally disappointing. “The result was not even a hint of protection,” Sparling wrote in a journal article last year.
In a potentially promising study, Peter Rice has been following the wives of men in China who contracted gonorrhea from other women. Although the wives have been exposed to the microbe, a third of them don’t become infected; Rice suspects that some in this group may produce an antibody against a certain sugar on the microbe’s surface, which might provide the basis for a vaccine. But, Sparling notes, because the gonococcus naturally infects only human cells, a gonorrhea vaccine will be difficult to test on animals. “I am still optimistic that a gonococcus vaccine is possible,” Sparling told me. “But it suffers from lack of will and money. Certainly, the time has come to get serious about this.”
In June, the World Health Organization issued a Global Action Plan against drug-resistant gonorrhea, offering a long list of recommendations, many of which are already being followed in the U.S. and Europe. One was a call for more drug research and development. The report also encouraged early screening of patients and educating them about the risks of the disease. The main concern is identifying drug-resistant strains as they emerge and reporting them to public-health authorities, so that the recommended treatment can be changed, if necessary.
This summer, I visited the walk-in clinic at Fenway Health, a community health center housed in a modern building on Boylston Street, in Boston. People often go to a walk-in clinic to be tested and treated for sexually transmitted infections, either because they don’t have a primary-care doctor or because they prefer the anonymity. This makes clinics ideally suited to identifying emerging superbugs. Fenway Health sees twenty thousand patients a year, about half of whom are lesbian, gay, bisexual, or transgender, and keeps extensive electronic records. Thanks to state-government support, anyone without insurance can drop in to be evaluated for free. That afternoon, one of the patients was a man in his late twenties who wasn’t sure that he was gay but, he said, had become addicted to sex with men. In the past year, he’d had more than forty anonymous encounters, arranged through Craigslist or a smartphone app. Marcy Gelman, a nurse practitioner, took a urine sample and two swabs, one from his throat and the other from his rectum, and sent them to be tested.
There are two kinds of tests for gonorrhea. One involves culturing the bacterium in a slurry of hemoglobin, amino acids, and vitamins, which reveals the specific strain of the gonococcus and the drugs to which it is more or less susceptible. It is a laborious process, and most clinics have abandoned it in favor of a DNA test that rapidly indicates whether the patient has gonorrhea, but not which variety. Fenway Health is the rare clinic that regularly performs both tests; public-health officials depend on it as a surveillance outpost for tracking the spread of gonorrhea. Other clinics have the option of sending specimens to state labs to be cultured; the results are factored into the C.D.C.’s Gonococcal Isolate Surveillance Project, which tracks antibiotic resistance in gonorrhea in the U.S. But many clinics have been closed in recent years owing to budget cuts, and few public-health labs test for antibiotic resistance.
“Both in terms of recognizing the problem when it emerges and dealing with it once it arrives, clinicians and the larger health-care community are getting to a cliff here,” Dr. Judith Wasserheit, an expert in sexually transmitted diseases at the University of Washington and the author, with Bolan and Sparling, of the recent New England Journal of Medicine article, told me. “Gonorrhea is doing again what it does so well—it’s getting ahead of us. What’s changed is that we don’t have a drug, and we have dramatically reduced the capacity to recognize, on a routine clinical basis, when resistance emerges.”
The primary hope for stemming the expected epidemic of resistant gonorrhea lies in persuading people to alter their behavior. “The public doesn’t really understand the links between gonorrhea and infertility, or that gonorrhea means an increased risk of acquiring H.I.V. and transmitting the virus,” Wasserheit told me. She added, “If your alternatives are vaginal sex, anal sex, or oral sex, most people feel like oral sex is the safest of the three. And, you know, in some ways they’re probably right.” Still, Wasserheit said, “it’s important to communicate that oral sex is not necessarily safe sex.”
The first educational message, Bolan told me, “is to use condoms correctly and consistently,” because this is known to reduce transmission. The next step is to promote condom use not only for vaginal and anal intercourse but also for fellatio. That will be a challenge, as public-health experts concede. Of the dozen patients I saw being screened during my visit to Fenway Health, not one had used a condom for oral sex.
Fenway identifies the most high-risk carriers—crystal-meth addicts, people with multiple partners—and tries to persuade them to abandon unprotected sex. At the clinic level, safe-sex education “is a kind of bargaining,” Dr. Kenneth Mayer, an infectious-disease expert who oversees Fenway’s research program, told me. “You’re trying to get the person to the next place”—to where talking about the necessity of using condoms during oral sex is even plausible. Dr. Stephen Boswell, the president and C.E.O. of Fenway Health, added, “It’s a tradeoff if your goal is to protect somebody from acquiring or transmitting H.I.V., and you are really trying to use a condom every time you have anal sex. But saying to somebody, ‘Use a condom every time you have oral sex,’ we don’t think that is necessarily going to be tenable.”
This summer, I also visited the Boston Medical Center, which draws from some of the city’s poorest neighborhoods; in the past year, nearly twenty-five hundred patients were tested for gonorrhea. Over the years, Faye Huang, a nurse practitioner, has seen high-school students, eighty-year-olds, prostitutes, men cruising for men, as well as what Huang calls the “worried well”—patients who have had limited or bad sexual experiences and are “constantly worried that, even if the condom was on, they might have gotten something.” Recently, a twenty-four-year-old Indian man had come in after noticing some swelling at the tip of his penis. He had had only two partners in his life: a woman in India and another in the U.S., with whom he had not used a condom. Huang got a urine specimen and drew blood to test for syphilis and H.I.V. “You never know,” she said. The urine test came back positive for gonorrhea. Huang gave him the C.D.C.’s recommended treatment: a shot of ceftriaxone and tablets of azithromycin. When he declined her suggestion that his partner be informed, she referred his case to Mark Thacker, a disease-intervention specialist with the Massachusetts Department of Public Health.
Soft-spoken and with the build of a football player, Thacker tries to cajole patients who test positive for gonorrhea into letting him notify their sexual contacts. He starts by discussing their social and medical history, and talking about the disease, then asks about the partners the infected person has had in the past sixty days. When one man couldn’t remember the screen names of his anonymous partners, Thacker took out his BlackBerry and offered to go online and try to pull up their profiles. “We actually show them pictures and get a little graphic, to get some leverage and, hopefully, coax them to be a little more compassionate about what might happen to the other person,” Thacker said. Only about half of the infected people he approaches readily divulge information about their sexual contacts. “A lot of people take it very, very lightly,” Thacker said. “ ‘Yup, I’ll just go get the shot, I’ll just take these pills, and I’ll be fine.’ ”Pursuing a case can take hours, as Thacker contacts doctors and nurses to request the release of information, then waits for return calls and follows up with the patients who have not been treated. Sometimes he drives out to the infected person’s home and takes him or her to a clinic for treatment. He routinely gives people his cell-phone number. In Massachusetts, there are as many as four thousand cases of gonorrhea each year to track, and only five disease-intervention specialists like Thacker. “We are caseworkers, case managers, and counsellors. You have to wear quite a few different hats to really do this work.” But, he said, “we are not the sex police.”
In the early nineteen-eighties, as a physician at the U.C.L.A. Medical Center, I cared for some of the first people diagnosed with AIDS. The disease was horrific, an unrelenting series of infections that filled lungs, inflamed bowels, and destroyed the brain. Yet it took years for sexual practices to change. Condoms, long dismissed as unnecessary for birth control and suboptimal for pleasure, ultimately returned as a proven way to stem the spread of H.I.V. The challenge now facing the public-health community is how to persuade people to rethink an insidious disease—and, to a great extent, a sexual practice—that has come to be viewed as trivial. As the distinction between safe sex and safer sex becomes ever less meaningful, the responsibility to be vigilant grows more personal, and more urgent. ♦
Read more http://www.newyorker.com/


Thanks for sharing with us. Akums Drugs has acquired recognition among world-wide for offering confident quality tablets. We ensure that our tablets are firmly screened on unique chemical structure before their final appearance. Antibiotic tablets
ReplyDeleteGood information.
ReplyDeletegonorrhea early symptoms
gonorrhea how do you get it